Sarah, an Area Support Coordinator at the Association, talks candidly about her own caring experience after her mum, Norma, was diagnosed with MND. Sarah recounts how her mum's symptoms progressed rapidly and highlights the challenges of communicating with a loved one in a hospital setting. Throughout the conversation, Sarah discusses the importance of communication and mutual support when navigating the challenges of MND.
Life before MND
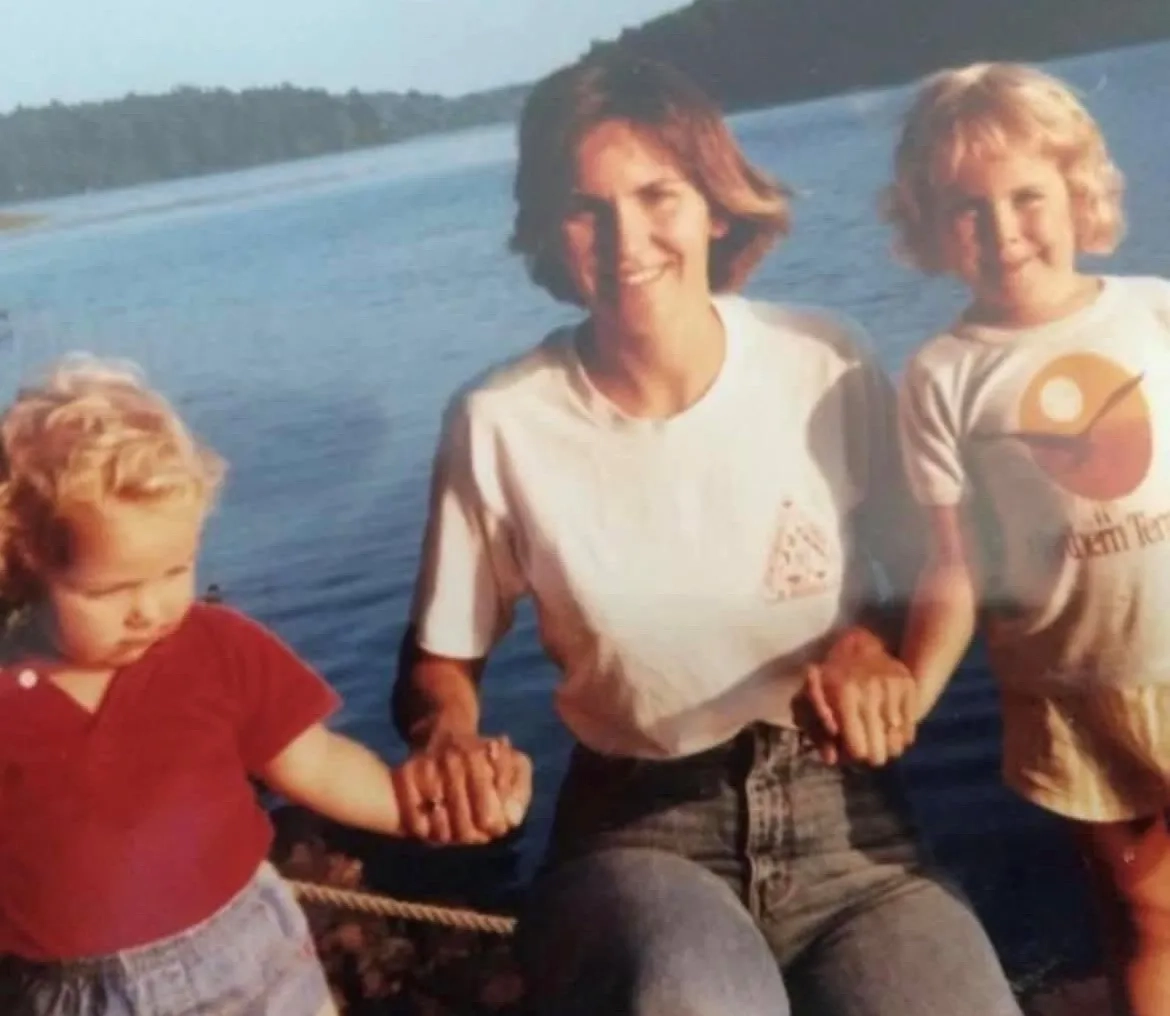
"It never occurred to any of us that anything bad would happen."
We did a lot together as a family and my mum was the glue that held it all together. We went on family holidays and my mum loved big family get-togethers. We all enjoyed being together and we were close knit. Mum belonged to a choir, which she loved. She also did a lot of walking, went to a lot of concerts and loved to travel. Just before she was diagnosed, she had gone to New Orleans on a jazz tour. She had a lot of friends, a very active social life, and enjoyed spending time with her children
I got married the year before she was diagnosed, and my sister was engaged and planning her wedding. My mum, my sister and I were very close, and we spent a lot of time together. It never occurred to any of us that anything bad would happen. It's just not something that ever enters your mind.
Early symptoms and diagnosis
"She came to the conclusion very early on that she had MND."
The first thing was her foot. She was really bothered about it, but we were convinced that she had a trapped nerve or something else relatively straightforward. We reassured her but she was clearly very worried about it, and my mum had a medical background, so she started Googling her symptoms because that's human nature, isn't it? She came to the conclusion very early on that she had MND.
She was diagnosed in August 2018. She went to her GP first, had multiple tests and was then referred to the neurologist who diagnosed her. Everything happened quickly following the diagnosis. I can remember going onto the internet, finding the Association website and calling the Connect helpline the day after she was diagnosed.
Mum had to leave work as an ODP for the NHS working in operating theatres quite soon after her diagnosis. Due to the physical nature of her job, it became impossible for her to do. Leaving work was hard for her because she wasn't leaving on her own terms because physically, she couldn't do it and that is very different to making the decision yourself. Mum had worked at the hospital for over 25 years and was leaving a group of incredible friends and colleagues, a support network.
Adapting to MND
"It was so devastating for her, and she just changed."
Almost overnight it went crazy. It is hard to say but my mum did not deal well with the diagnosis. There is no good way of dealing with a diagnosis like that, but we lost mum the day she was diagnosed. It was just too much. It was so devastating for her, and she just changed. It seemed like overnight multiple professionals were suddenly in our lives. You go from having a normal life and a normal house, then suddenly the phone never stops ringing and people are coming and going all the time. That increased as the disease progressed to the point where the house was like a hospital. It’s quite overwhelming to get your head around but despite the intrusion, the team my mum had were brilliant.
Association support
"We were all dealing with such a huge shock, and we were all so lost."
Initially, the Association sent an Association Visitor (AV) round, and she was fantastic. I don't really know what we would have done without her. She supported not just my mum, but me, my stepdad, my sister, and my stepsister as well. She understood not to push my mum because my mum really didn't want to know more than she needed to know or what the next phase would be. We were trying to be there as much as we could to support her, but we were all dealing with such a huge shock, and we were all so lost. That is where my mum's AV was so helpful because she came in and scooped us all up and put the light on.
My sister and I had counselling arranged by the Association through the local hospice, but my mum declined all counselling. She got to a point where she didn't want to talk about MND anymore.
Progression of MND and moving home
"She looked so happy to feel running water on her skin. That day she smiled."
It was all very rapid. It started in her foot and just seemed to spread like wildfire. It was almost as if something changed every week. We would be trying to get our heads around the latest change, and then something else would change. She initially had a support brace on her ankle and then very quickly she had to have a stick, then a walker, then a manual wheelchair, then a mobility scooter and then an electric wheelchair.
They decided to go ahead with the move to the village they had always wanted to live in but now suddenly, the considerations they had to make in buying a house were very different. They were having to think about how accessible it was and whether they could install a wet room and whether the doorways were wide enough to accommodate an electric wheelchair. There were months where she couldn’t have a shower because the wet room hadn't been installed yet. We were having to do strip washes every day. I remember the first time she had a shower after the wet room had finally been installed and she sat under that shower for so long. She looked so happy to feel running water on her skin. That day she smiled.
It felt like I blinked and suddenly she was in an electric wheelchair, had lost her voice, and could no longer eat and had a PEG fitted. It felt rapid and it was two years from diagnosis to when she died. She was diagnosed in August 18, and she died in August 20.
Admitted to hospital
"There were a lot of problems with communication whilst she was in hospital."
My mum was admitted to hospital twice during COVID. Initially, when she went in, we weren't allowed to visit at all. It was awful.
The second time she went into hospital she had lost her voice completely and the care she received at the hospital wasn't good. Her basic care needs were not being met because they didn't have the capacity to do it, or the knowledge of MND specific care needs to make sure that her mouth care was done properly, or she was repositioned properly. You often see a decline in MND patients after they have gone for a stay in hospital because there is not the same level of MND specific care. I remember going in to see her and they hadn't done her mouth care, and her mouth was almost sealed shut. When she was at home and being cared for by us, we would never have let that happen. You can always care for someone better when they are your loved one and you would do anything for them. To see her so vulnerable was incredibly hard.
There were a lot of problems with communication whilst she was in hospital. I find this a lot in my role with the Association. I get calls from people because their loved one is in hospital, and they are dealing with nursing staff who may have never met someone with MND before throughout their whole career.
Caring for MND
"Seeing her so vulnerable and unable to do the things she once loved was heartbreaking."
Watching someone you love living with MND, you feel powerless. Nobody tells you how to care for someone, what you need to do or how to do it. You are essentially left to it. We never had any formal training on manual handling, we just worked it out as we went along. It was trial and error initially. I worry that there are a lot of people who are caring for someone who don't want to be caring, maybe it's not in their nature or it’s too emotionally hard and they feel resentful. Many people don't have a choice because it so expensive to get carers in or they don't qualify for CHC funding.
Being a carer is physically hard because of the lifting and the manual handling, but then there is the emotional drain. The emotional side of it is tough. Seeing her so vulnerable and unable to do the things she once loved was heartbreaking. Mum’s day would begin with being hoisted out of bed in the morning, showered, brought downstairs, hoisted into the riser recliner, and there she would remain until she was hoisted back to bed. We looked after her alone to the best of our ability for as long as we could, but it got to a point where her care needs were too great. Thankfully mum was granted CHC funding because the care she required would have cost thousands of pounds. The carers were lovely, and we all became close, they were like part of the family. They could get a smile and laugh out of mum sometimes when we couldn't. They adored her and were devastated when she died.
Life after MND and working for the Association
"Why would I want to work anywhere else?"
We had spent two years caring for mum, running around the house, assisting the carers, going in and out of hospital and meeting with the endless list of professionals. Then suddenly, it all stopped, and it was quiet, and she was gone. We felt lost. We have created a new normal and it's obviously not like it was when mum was alive, but we have tried our best to keep things going, to keep up the traditions that were so important to her. I don't think there is a single day that goes by where I don't mention her to my children, and I know it is the same for my sisters. Despite not being here, my mum is still very much a part of our family. We were right when we said she was the glue that held it all together because it took us a long time to pick ourselves back up.
We felt incredibly supported by the Association. That is why I am here and doing the job I do. Why would I want to work anywhere else? It has been helpful in my day-to-day job, understanding what it is like to live with MND and the effect it has on not just person with MND, but those around them. I have so much empathy for the people I work with because I have been in that situation myself, I have seen it play out and it is horrendous.
Back to Global MND Awareness Day webpage