GPs and others in the primary care team can make a great difference to the quality of life of people with MND, with timely care, support and symptom management.
Whether you are a GP, nurse or other member of the primary care team, this information gives practical tips on the care of someone with MND, and the role you and your team can play.
Looking for all our resources for a specific profession or topic, for you and the people you support?
Use our Professional Information Finder
Diagnosis of MND
The importance of timely diagnosis
Rapid and accurate diagnosis, performed by a medical doctor experienced in MND care, usually a neurologist, is crucial in ensuring the needs of people living with MND are met from the earliest possible stage.
Quality of life for people with MND may be improved by:
- accurate recognition of the condition
- explanation of the likely progression of symptoms within a supportive therapy team
- prompt introduction of appropriate treatments and interventions.
How MND is diagnosed
There is no single diagnostic test for MND. Diagnosis is based on features in the clinical history and examination, usually accompanied by electrophysiological tests, which will include EMG and nerve conduction studies.
Other tests may include:
- MRI scanning of the brain and spinal cord
- various blood tests
- lumbar puncture
- muscle biopsy.
The purpose of these tests is to exclude the presence of other neurological conditions, with particular focus on those with treatments likely to be effective if administered early. In the early stages of MND, symptoms can be similar to those seen in other conditions, so people may spend months seeing various specialists and undergoing unsuccessful treatments until MND is suspected.
Red Flags Diagnosis Tool
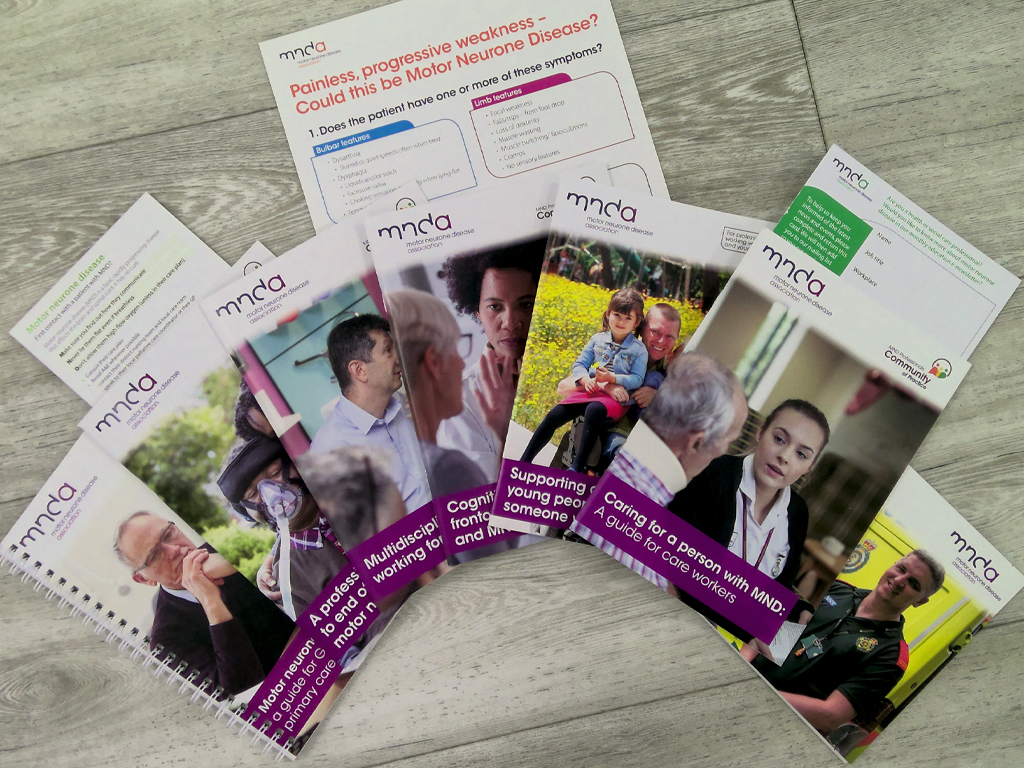
The MND Association's Red Flag tool for GPs, produced in partnership with the Royal College of General Practitioners, is designed to improve timely referrals to neurology and therefore speed up the time to accurate diagnosis.
Support after diagnosis
When someone is diagnosed with MND they may take time to adjust and come back with questions some time after. It is important they have suitable support at this stage, including a point of contact to return to with questions and access to appropriate information.
GP management of MND
Working with the specialist team
Where a person with MND is being seen regularly by a neurologist, a shared-care approach may be agreed between the neurologist and GP. This is particularly important where the neurologist is based some distance away and access becomes increasingly difficult as the disease progresses.
The GP is responsible for liaising closely with and, in some cases, co-ordinating the professionals currently involved in the care of the person with MND. The GP may work in liaison with an MND care co-ordinator, who may be based in an MND care centre or network.
Onward referrals
While the primary healthcare team may be able to meet some of the needs of the person with MND and manage many of their symptoms, the input of other health and social care professionals is vital to the care and support of people with MND.
The GP may act as the gatekeeper to other services, referring to appropriate specialists in the multidisciplinary team.
Treatment for MND
Riluzole is the only licensed drug available in the UK that prolongs life. Clinical trials have shown that, on average, it extends survival by around three to six months if taken for 18 months.
Its benefit does not show in tests of improved muscle strength. Instead it seems to reduce, on average, the rate of decline of function in MND. People with MND who take riluzole should be made aware that they will not feel any stronger when they take the drug.
Generally a hospital consultant will assess a person’s suitability for riluzole and prescribe the first course of the drug.
After this, the GP and specialist should agree a shared-care protocol, under which the GP issues repeat prescriptions. In a few areas however, the prescribing and dispensing of riluzole is undertaken by the specialised centre throughout the patient’s illness.
Normal baseline blood test should be undertaken initially, then monthly full blood count and liver function test for three months, followed by three-monthly for the first year, and annually thereafter. Responsibility for prescribing and monitoring should be made clear in the protocol.
Riluzole is available in tablets in generic or branded form (Rilutek). A liquid form is also available (Teglutik), which may be easier for some people with MND to swallow.
Symptom management
Sometimes, when people are told there is no effective curative treatment for MND, they interpret this as meaning that nothing can be done. Some will struggle on without asking for advice and treatment for symptoms, which could alleviate discomfort. They should be encouraged to talk about the symptoms they have and the potential treatments and therapies available.
Key actions for GPs
Prompt referral for diagnosis
Use the Red Flag tool to recognise early signs of MND in order to refer to neurology in a timely manner.
Assessing needs
Use a person-centred approach to listen to and ascertain the physical, social, emotional and spiritual needs of the person with MND and their carers at each appointment.
Refer to appropriate specialist teams as necessary.
Monitoring symptoms
Monitor and assess symptoms, including signs of:
Respiratory involvement – early signs should trigger referral to the specialist respiratory team.
Cognitive change – this has implications for decision making and future management.
In collaboration with consultants in neurology and palliative care, initiate appropriate management and treatment, including anticipatory symptomatic intervention.
Support and information
Provide support and information before diagnosis and throughout the course of the disease.
Advise on the need to inform the DVLA or DVA of MND diagnosis.
Complete a DS1500 form to support a benefit application.
Repeat prescriptions for riluzole
Issue repeat prescriptions if the person with MND is prescribed riluzole by their neurologist: a shared-care protocol should be agreed.
Palliative care
Include the person with MND on local palliative care registers/lists/co-ordination systems, where these exist – eg the Gold Standards Framework, Electronic Palliative Care Co-ordination Systems (EPaCCS).
Advanced care planning
Help the person with MND to talk through management options, including end of life decisions and Advance Decisions to Refuse Treatment (ADRT), as early as possible.
See our information on palliative and end of life care.
Checklist
Can you identify the person with MND as having a neurological condition on your practice IT system?
If no: Use the appropriate coding so your system flags when the person contacts the surgery and the appropriate response can be given.
Is the person’s care regularly discussed within the primary healthcare team (PHCT)?
If no: Put the patient’s name on the Supportive Care Register within your practice.
Is there a member of the PHCT who has been nominated as the co-ordinator of the patient’s care?
If no: Identify a named person who acts as the single point of contact within the PHCT and can liaise with all health and social care professionals involved in the person’s care.
Are efforts being made to control all symptoms currently being experienced by the person with MND?
If no: Look at options for management. If symptoms are still uncontrolled, refer onwards.
Is it flagged with the out-of-hours service provider that this person has MND?
If no: Notify your out-of-hours service provider and ensure access is given to all relevant facts/wishes.
Are plans in place for emergency care provision if the person’s carer cannot support for any reason?
If no: An assessment of care needs should consider this. Refer to social services.
Do you have a copy of any existing DNACPR order/ADRT/advance care plan/preferred place of care request in your practice records?
If no: Ask to keep a copy in your patient records.
Is the ambulance service aware of any DNACPR order/ADRT/preferred place of care request?
If no: Notify the ambulance service so it can be flagged on its system to prevent inappropriate care or treatment.
Are you aware of the name of the main carer for this person?
If no: Record the name of the main carer and their contact details on your practice system.
Is the carer is registered with your practice, is their record cross-referenced on your system?
If no: Put a flag on the carer’s record so you are aware of any potential impact on the carer’s health.
Do you know what the patient’s wishes are in relation to end of life?
If no: Use active listening skills to clarify these as the opportunity presents.
Have end of life wishes been recorded, so other members of the PHCT are also aware?
If no: Encourage the patient to record their wishes and make other members of their family and the PHCT aware.
Page last updated: July 2023
Next review: July 2025